PPP: Second Round of Funding Appears More Appropriately Managed
May 4, 2020
Signia Unveils New “Mask Mode” Feature
July 31, 2020“The jury is now in” on potential for transmission during otolaryngology procedures
by Molly Walker, Associate Editor, MedPage Today, July 23, 2020
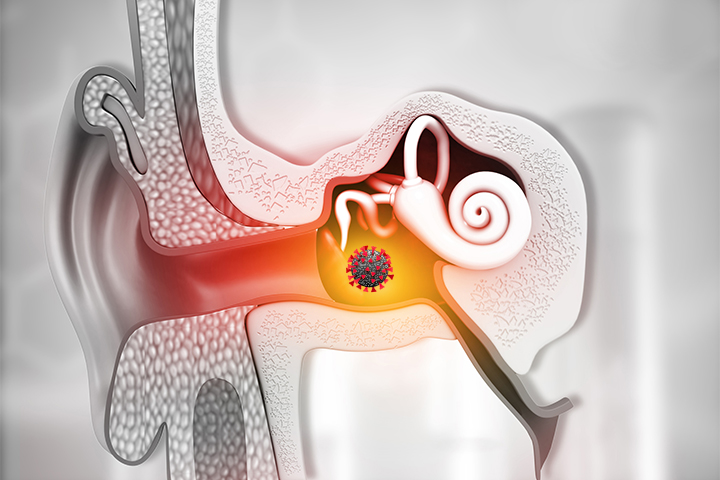
SARS-CoV-2, the virus that causes COVID-19, was discovered in the middle ear and mastoid during autopsies of patients with COVID-19, researcher found.
Autopsies of two of three patients who died with COVID-19 tested positive for SARS-CoV-2 in the mastoid or middle ear, with virus isolated from two of six mastoids and three of six middle ears, reported C. Matthew Stewart, MD, PhD, of Johns Hopkins Outpatient Center in Baltimore, and colleagues.
The authors, writing in JAMA Otolaryngology — Head & Neck Surgery, noted this study has “significant implications for otolaryngology procedures.”
“Similar to procedures of the nose, mouth, and airway, droplet precautions during ear surgery are warranted for patients with COVID-19 owing to risk of infection to health care personnel,” they wrote. “Droplet precautions (including eye protection and proper N95 level mask) are warranted for outpatient procedures involving the middle ear due to proximity to these potentially infectious spaces.”
Bradley Kesser, MD, of the University of Virginia in Charlottesville, trumpeted the findings as “News flash!” in his accompanying editorial.
“Otolaryngologists (especially otologists and/or neurotologists) around the globe have been waiting 6 months for this study,” he wrote. “The jury is now in.”
Kesser explained the anatomic connection between the nasopharynx, as the site of initial infection for SARS-CoV-2, to the tympanic membrane and the eustachian tube, which raised the question if the virus could gain access to the middle ear space and “put health care workers at additional risk.”
While he added no report has documented COVID-19 infection in a healthcare worker as a result of a middle ear or mastoid procedure, “mastoidectomy clearly generates aerosols and exposes health care workers.”
“Suctioning the middle ear through a tympanic membrane perforation, intratympanic injections, and mastoid cavity debridement (especially if the cavity is exposed to the eustachian tube) may carry the risk of aerosolization and transmission of SARS-CoV-2,” Kesser wrote.
He added this has implications for ambulatory clinics and office settings as well, recommending patients be pre-screened a day or two before the office visit, along with in-office screening the day of and reducing the waiting room population to ensure adequate social distancing.
Stewart and colleagues examined three deceased patients — a woman in her 80s and a man and woman in their 60s. Autopsies were conducted 48 hours and 16 hours after death in the patients who tested positive, and 44 hours after death in the patient who tested negative.
The authors noted the post-mortem interval prior to autopsy as a main limitation to the study, and that one patient who tested positive in one ear only was autopsied 48 hours later, while the autopsy was performed 44 hours after death in the negative case. They also added there were “limited” conclusions, particularly for asymptomatic carriers.
Finally, they noted colonization of the middle ear and mastoid with SARS-CoV-2 “does not necessarily imply current or future otologic symptomatology,” and said that living patients with COVID-19 may benefit from screening for otologic manifestations of the virus.
Stewart’s group suggested that future studies with in vivo samples during routine ear surgery could help quantify the incidence of viral colonization in living COVID-19-positive and COVID-19-negative patients.
Original article link: https://www.medpagetoday.com/infectiousdisease/covid19/87720